Hot flashes and night sweats are among the most infamous menopause maladies. But you might want to pay attention to your teeth and gums, too.
“I’m not sure that people are aware of this,” said Dr. Thomas Sollecito, chief of oral medicine at the University of Pennsylvania.
Hormonal changes — mainly a sharp drop in estrogen — can reduce bone density and saliva production and harm your gums. All of that can affect your teeth.
Oral care experts say there are ways to counteract these effects and keep your menopausal mouth healthy.
Menopause happens when a woman goes 12 consecutive months without a menstrual period. But some of the hormone-related dental problems may begin during perimenopause, when the ovaries gradually make less estrogen, said Dr. Maiara Hister-Cockrell, a dentist with the University of Texas Health San Antonio.
One of the biggest concerns is less saliva, which Sollecito called “one of the most important fluids in our body.”
When the saliva flow slows, it can cause dry mouth, which brings a greater risk of mouth soreness, oral yeast infections and cavities. Those risks are even higher when people take medicines for high blood pressure or diabetes that can also cause dry mouth, Hister-Cockrell said.
Less saliva also means less of its bacteria-killing enzymes and tooth-strengthening minerals, said Dr. Sally Cram, a periodontist in Washington, D.C.
When your mouth is dry, she said, “those bacteria are proliferating and you’re more prone to get tooth decay.” And if decay festers, tooth loss is possible.
Decreasing bone density and receding gums exacerbate these problems. If the socket that holds the tooth is less dense, Sollecito said, it’s more vulnerable to bone loss. And gum recession can leave some tooth surfaces without the enamel that protects them from cavities.
Women in this phase of life are also more likely to develop periodontal disease, when plaque and bacteria collect under gums and around teeth.
“Gum tissue starts to get red and swollen,” said Cram, a spokesperson for the American Dental Association. “It bleeds and it starts pulling away from the teeth, creating deeper crevices around the teeth that are clearly harder to keep clean.”
Some people experience “burning mouth syndrome.” Hister-Cockrell said a burning sensation can extend to the tongue, palate and lips.
“As you could well imagine,” Sollecito added, “this could all really spiral out of control.”
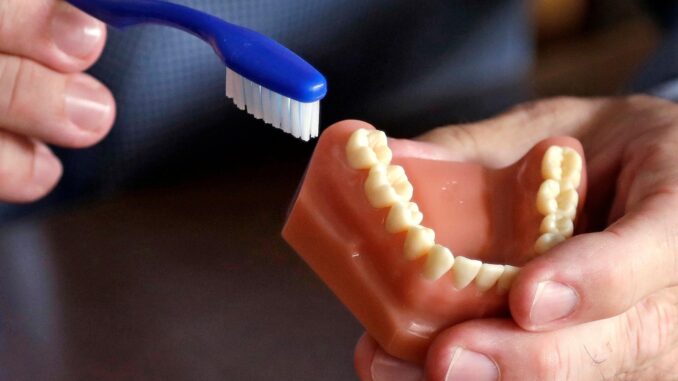
The first line of defense, experts said, is good oral hygiene and nutrition. Eat a balanced diet low on sweets and high on calcium-rich foods. Brush carefully with fluoride toothpaste at least twice a day and floss regularly.
“An electric toothbrush can be more helpful than manual toothbrushing,” Cram said. “See your dentist regularly and ask them: Am I doing a good job? And if I’m not, what could help me do a better job?”
Patients should also ask their dentists whether they should be seen more than twice a year, as well as consider in-office fluoride treatments to strengthen the surface of their teeth and prescription high-fluoride toothpaste.
At home, experts said, treating dry mouth is a priority. So stay hydrated.
“None of us really probably drink enough water throughout the day,” Cram said.
People can also use over-the-counter dry mouth sprays, lozenges or rinses. In severe cases, Sollecito said they can ask their dentist about prescription medications that increase the amount of saliva in the mouth but come with side effects. There are also prescription medications for burning mouth syndrome.
“The bottom line,” Cram said, “is most oral conditions and problems during menopause are totally preventable” by paying attention, taking good care of your teeth at home and regularly going to the dentist.
___
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.


Be the first to comment