
 Pete Middleton
Pete MiddletonPete Middleton, who lives in Northamptonshire, UK with his wife, has long been an early adopter of technology.
He became interested in computing while in the Royal Air Force in the 1980s and went on to learn several programming languages.
In recent years he’s been enthusiastic about the rise of AI, which he uses for editing photographs, for translating text messages, and for research.
Overall, Mr Middleton is having a busy retirement. In addition to his hobbies and his dementia blog, he’s a lived-experience consultant, committee member and volunteer with Alzheimer’s Society.
Since his diagnosis with dementia five years ago, at the age of 65, he’s noticed changes to his short-term memory. For example, “I can still write apps for mobile phones, but I can’t remember where I put my telephone.”
Mr Middleton believes that AI could help to bridge this gap.
“If people incorporate the benefits of using AI into their lives, it will be good for their self-respect and self-esteem, and it will keep them independent for longer. And if it does that, it keeps them out of the NHS system and out of care homes.”
A number of AI-based tools offer to help with the daily routines of people living with dementia.
One is Simon, an app that uses geo-tracking and machine learning to determine the specific needs of a user and provide notifications that could help.
“For example, this could include reminding individuals of a PIN when the app detects they are at the bank,” says Fiona Carragher, the director of research and influencing at Alzheimer’s Society. Simon is currently being beta tested.
A long-running programme in this domain is the Florence Project. The Florence Project seeks to develop useful communication technologies for people living with dementia.
“We’re looking at this issue of keeping communication strong – so, not replacing communication between family and carers and people living with dementia, but rather supporting it,” says Janet Wiles, a professor in human-centred computing at Australia’s University of Queensland.
 The Florence Project
The Florence ProjectProf Wiles, whose own mother lives with dementia, is part of a team working on the Florence Project.
The team are keen to avoid their products ending up in a drawer of unused, overly complicated devices.
So, it includes a Living Experience Expert Panel, made up of people living with dementia and those who help care for them.
The project has developed three devices – a diary, a music player, and a digital photo screen. These are easy-to-use, single-function devices with physical elements like knobs or buttons, which also integrate the preferences of the living experience experts.
The content on the devices can be adjusted either locally or remotely. For instance, a relative in another part of the country can update the playlist on the music player, if the person living with dementia gives permission.
AI helps with personalising these tools. A knowledge bank is built for each person, based on questions they answer or conversations they have. Audio is transcribed and in some cases translated, before feeding into the kinds of information that are made available on the devices.
For example, the diary device might display the photo of a new part-time carer next to the time that they will arrive.
Needs and preferences may change as their condition does. So, for example, the information in the diary can be simplified to match the needs of the user.
The team were keen not to rush the development process – the project has been running for about a decade already, and is now at the stage of testing its prototypes.
“The downside for tech that goes wrong for people with dementia is often way worse than it would be for other people,” Prof Wiles cautions.
She emphasises that data privacy and security are especially important for people with dementia.
 Christine Ro
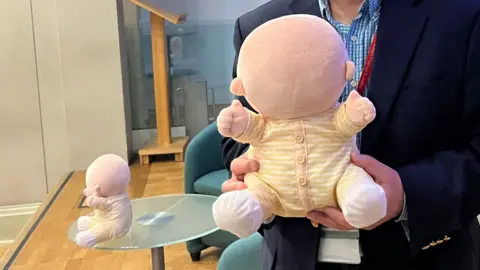
Christine RoAI-based chatbots are also being integrated into companion robots. Hiro-chan is a faceless, huggable, soft therapy robot; the researchers believe that interacting with Hiro-chan reduces stress in people with dementia.
They’re now working on integrating ChatGPT into the robots, along with speakers and microphones. The total weight would remain less than 800 grams.
In initial tests with people with dementia living in care homes, “we found that a simpler dialogue than we expected would be more engaging for more of them,” says Hidenobu Sumioka, a roboticist at Advanced Telecommunications Research Institute International in Kyoto.
However, “it’s critical that AI doesn’t replace the human contact that is so important in dementia care,” Ms Carragher says. “Instead, it should be used to enhance care in a way that is beneficial to people living with dementia and their carers.”
Dennis Frost, a retired programmer who has served on the Florence Project’s Living Experience Expert Panel, points out that social engagement is very important for people who are diagnosed with dementia.
“I would suggest increasing human interaction should be a priority over increasing AI interaction. After all would an AI actually care if I lived or died?”
Mr Middleton sees great promise in AI, but emphasises that any technologies intended for people with dementia must be customisable to a diverse set of people.
“No two people with dementia are the same,” Mr Middleton says. “What works for me won’t work perhaps for my next-door neighbour, who has dementia.”
“So developers must be very careful when they’re developing products to not just target the dementia community in general, but look for the specific stages of dementia and try and make up match up what they do with the person’s ability.”



Be the first to comment